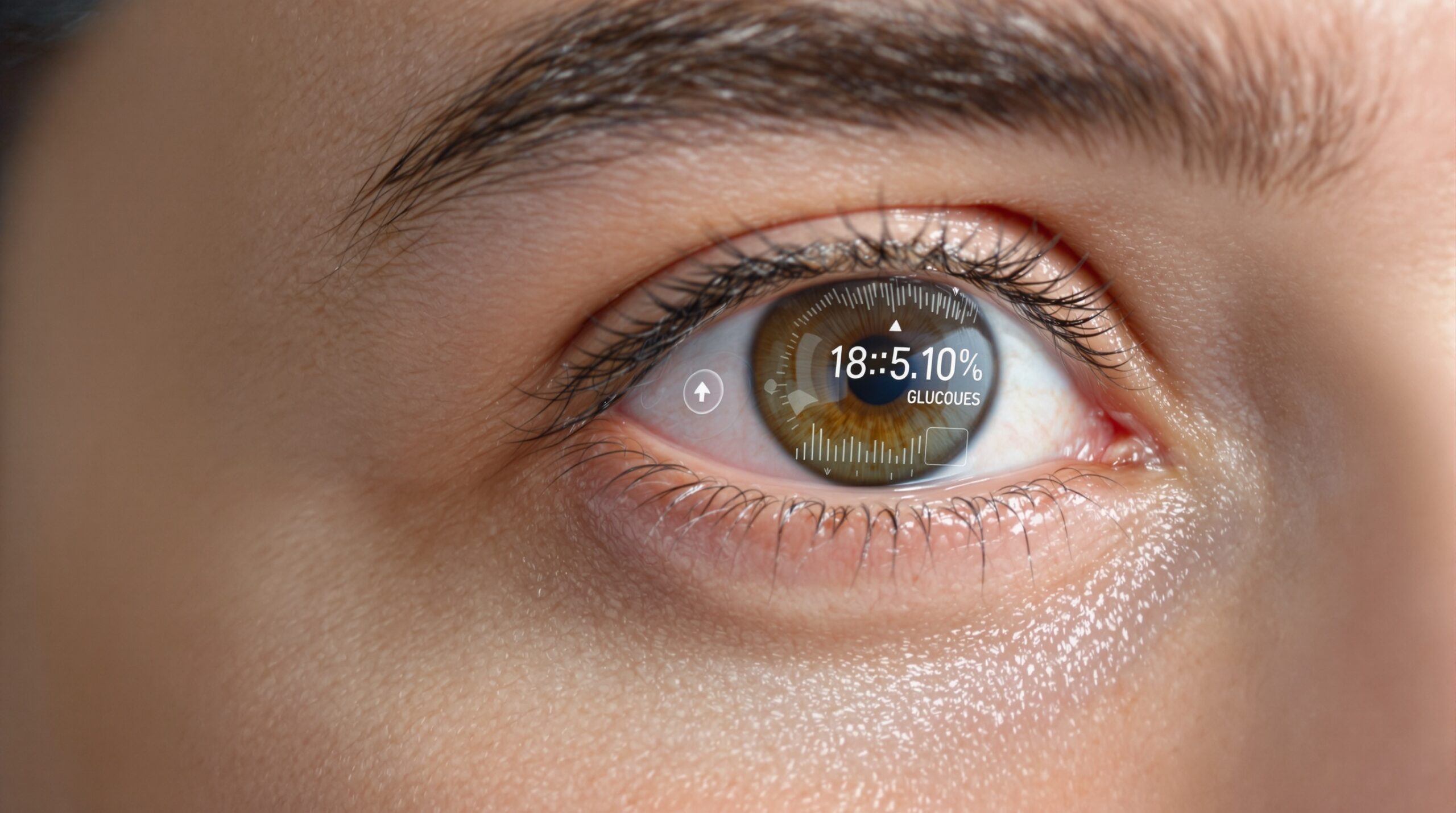
Researchers have publicly demonstrated a battery-free smart contact lens that monitors glucose in tears continuously. The lens transmits readings to nearby phones, enabling real-time tracking without an implanted sensor. The debut highlights progress in noninvasive glucose monitoring and wearable bioelectronics.
The prototype shows how passive electronics can fit inside a soft lens and still function reliably. It relies on wireless power and communication rather than a miniature battery. This design choice reduces thickness, heat, and long-term safety concerns.
A Battery-Free Breakthrough for Ocular Biosensing
The lens harvests energy from a phone or dedicated reader using near-field communication. That harvested energy powers a tiny sensing circuit embedded within the lens material. The circuit then sends data back to the phone using the same link.
How the Smart Contact Lens Works
The device integrates an electrochemical glucose sensor into a medical-grade hydrogel contact lens. A micro-antenna encircles the lens periphery and couples to a smartphone’s NFC field. An ultralow-power chip rectifies energy, controls sensing, and backscatters data securely.
The glucose sensor typically uses an enzymatic layer that reacts with tear glucose molecules. That reaction produces an electrical signal proportional to glucose concentration in the tear film. The chip samples the signal at set intervals and encodes it for transmission.
The entire stack remains transparent in the optical zone to preserve vision. Components sit within the lens rim to minimize visual artifacts and discomfort. The soft lens maintains oxygen permeability, hydration, and tear exchange for corneal health.
Tear Glucose Offers Promise, With Important Caveats
Tear glucose can reflect systemic glucose, but the relationship is complex and variable. Concentrations in tears are lower than in blood and can lag during rapid changes. Environmental factors and tear dynamics can also influence measured values.
Researchers acknowledge these scientific challenges and design the system to support calibration. The app can guide users through calibration against fingerstick or established devices. Such workflows aim to improve trend accuracy and reduce individual variability.
Verily halted a well-known glucose lens project in 2018 due to correlation concerns. Newer designs use improved sensors, electronics, and algorithms to address those limitations. Still, clinical validation remains essential before any clinical claims are justified.
Data Syncing and Smartphone Integration
The lens communicates with phones through NFC, which most modern smartphones already support. Users can periodically hold the phone near the eye for data retrieval. A lightweight reader in eyeglasses could support more frequent or automatic syncing.
The companion app displays real-time readings, trends, and customizable alerts. It stores data locally and can sync to secure cloud services when authorized. Users can share summaries with clinicians, caregivers, or research programs as they choose.
End-to-end encryption protects data in transit and at rest. The system follows privacy principles, including user consent and transparent data policies. Such practices will be critical for trust and regulatory compliance.
Safety and Comfort Considerations
Eliminating a battery reduces thickness and removes a potential failure risk. The device operates within strict power limits to avoid heat buildup. Engineers test for electromagnetic safety and ocular tissue compatibility.
The lens uses biocompatible hydrogels common in soft contacts. Edges remain smooth, and embedded parts avoid the pupil and iris zones. Users still must follow standard lens hygiene and wear-time recommendations.
Power and Communication Design
The system typically uses the 13.56 MHz NFC band for power and data. Backscatter modulation enables the lens to transmit without a power-hungry radio. Duty-cycled sensing balances measurement frequency and comfort.
Practical range remains a few centimeters, consistent with NFC physics. That range supports intentional reads but prevents unwanted continuous tracking. It also helps limit power exposure and conserves harvested energy.
Early Testing and Validation Steps
Developers start with bench testing using tear simulants and controlled glucose solutions. They characterize response curves, drift, and interference from tear constituents. Temperature and pH effects also receive careful evaluation.
Animal studies can assess ocular safety, biostability, and signal behavior in a living system. Researchers then progress to small human feasibility studies for comfort and connectivity. Those studies also examine real-world motion, blinking, and dry-eye impacts.
Clinical trials must quantify accuracy against reference glucose methods. Investigators typically report metrics like mean absolute relative difference. They also assess lag times during meals, exercise, and insulin adjustments.
Comparison With Skin-Worn Continuous Glucose Monitors
Skin-worn CGMs use a tiny filament under the skin to measure interstitial glucose. They provide established performance, continuous streams, and broad clinical evidence. However, they require insertion and adhesive maintenance.
A contact lens avoids skin insertion and visible patches. It could appeal to users seeking a less obtrusive option. Yet, tear glucose behavior and practical wear time introduce different trade-offs.
Regulatory Path and Market Outlook
Any glucose-sensing lens requires rigorous regulatory review before clinical use. Developers must demonstrate safety, effectiveness, manufacturing quality, and cybersecurity. Timelines depend on trial results and agency feedback.
What to Watch Next
Observers should watch for peer-reviewed accuracy data across diverse user populations. Partnerships with major lens manufacturers would signal scale-up momentum. Regulatory submissions and pivotal trials would mark the next milestone.
The debut shows how far smart lenses have advanced since early concepts. It brings practical communication, safer power, and thoughtful app integration together. That integration narrows the gap between laboratory prototypes and everyday use.
Nevertheless, success depends on strong clinical evidence and transparent risk management. Developers must prove reliability across daily conditions, not only controlled settings. Users and clinicians need clear guidance on calibration and interpretation.
Health systems and payers will evaluate outcomes, adherence, and costs. If benefits match expectations, reimbursement can drive adoption. Otherwise, the technology may find niche use cases initially.
Interoperability will matter for long-term value. Open standards help integrate lens data with electronic health records and coaching tools. That integration can reduce data silos and improve care coordination.
Battery-free design also invites broader biosensing possibilities. Similar platforms could monitor electrolytes, lactate, or ocular biomarkers noninvasively. Each application would require targeted validation and tailored algorithms.
Supply chain capability will shape production scale and cost. Ultra-thin antennas, stretchable circuits, and high-yield encapsulation are critical. Partnerships can align specialized expertise across these domains.
Ethical considerations deserve continued attention. Transparent consent, data minimization, and clear sharing controls protect users. Independent audits can strengthen accountability for sensitive health data.
User experience will influence adherence and outcomes. Comfort, fogging resistance, and stable vision must match conventional lenses. Easy cleaning and intuitive app design further support daily use.
Training materials and clinician support can reduce learning curves. Pharmacists and diabetes educators can help interpret lens trends appropriately. Good support reduces misuse and frustration during adoption.
Importantly, the lens is not a replacement for medical advice. Users should consult clinicians for individualized decisions. The technology aims to complement professional care, not replace it.
As development progresses, the research community can share protocols and datasets. Shared learning accelerates improvements and facilitates independent replication. That collaboration benefits everyone from patients to innovators.
The new lens pushes wearable health sensing toward a lighter, safer future. Its battery-free architecture reduces risks while enabling continuous insights. With rigorous evidence, it could expand options for glucose monitoring.
Progress will require patience and careful testing. However, the debut marks a meaningful engineering milestone for ocular biosensing. The next chapters will determine its clinical and commercial impact.