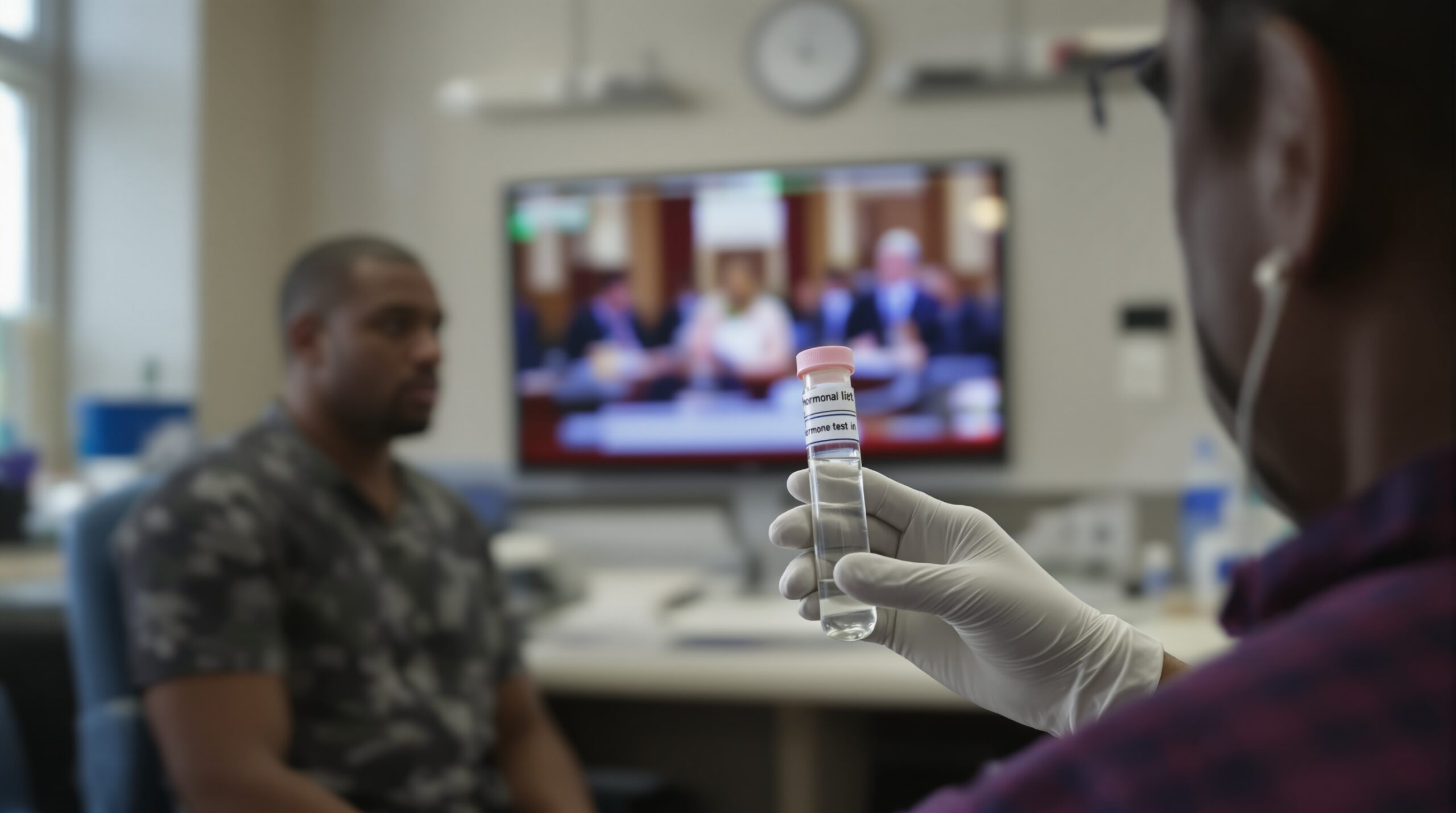
A new peer‑reviewed study reports an association between microplastic exposure and hormonal changes in adults. Researchers observed measurable differences in hormone markers among participants with higher exposure indicators. The findings raise concerns about endocrine health and broader population risks. The study’s conclusions now fuel an urgent and widening policy debate.
Policymakers face pressure to evaluate microplastics within existing chemical safety frameworks. Public health agencies consider surveillance, exposure reduction, and precautionary guidance. Industry groups urge balanced risk assessments and methodological rigor. The conversation is moving quickly across sectors and jurisdictions.
What the Study Found
The study linked higher microplastic exposure with altered hormone profiles across several endocrine axes. Differences appeared in markers related to stress, thyroid, and reproductive function. Associations persisted after adjusting for multiple lifestyle and demographic factors. The magnitude varied across subgroups by sex and age. These patterns suggest biologically meaningful effects that merit attention.
Measuring Exposure and Outcomes
Researchers assessed microplastic exposure using validated biomarkers and polymer‑related chemical indicators. Biological samples collected from participants captured internal exposure levels. The team quantified hormone concentrations with standardized clinical assays. Statistical models examined exposure‑response trends and tested potential confounders. Results indicated consistent associations across multiple analytic approaches.
Importantly, the study explored both direct particle markers and associated additive chemicals. This combined approach reflected the complex nature of real‑world exposure. It also improved sensitivity for detecting subtle hormonal differences. Together, these methods strengthened the credibility of the observed patterns. The analytical framework encourages replication in diverse cohorts.
Why a Biological Link Is Plausible
Microplastics can carry additives with known endocrine activity, including bisphenols and phthalates. Particles may also adsorb environmental pollutants and deliver them into tissues. Inflammation triggered by particles can disrupt hormonal signaling pathways. Oxidative stress may further alter endocrine feedback loops. These mechanisms create credible links between exposure and hormonal variation.
Endocrine systems often show nonlinear responses to chemical signals. Small exposures can produce measurable effects at certain developmental or physiological windows. Mixtures complicate predictions by interacting within shared pathways. The study’s associations align with these established toxicological principles. Such coherence supports cautious interpretation toward public health protection.
Strengths and Limitations
The study used pre‑specified protocols and blinded laboratory analyses. Researchers adjusted for diet, smoking, weight, medication use, and socioeconomic indicators. They conducted sensitivity analyses to test model robustness. Findings remained directionally consistent across these checks. These steps strengthen confidence in the reported associations.
However, the observational design limits causal inference. Exposure misclassification remains possible because measurements capture snapshots. Residual confounding cannot be completely ruled out. Longitudinal follow‑up would clarify temporal ordering and persistence. Replication across diverse populations remains essential for generalizability.
Endocrine outcomes can vary naturally across days and seasons. Medications and acute illness may influence hormone levels. The study addressed many factors but not all possibilities. These realities argue for careful interpretation and additional research. Policymakers should weigh evidence with both humility and urgency.
Public Health Stakes
Hormones regulate metabolism, reproduction, mood, and cardiovascular function. Even small disruptions can produce population‑level health shifts. Vulnerable groups may face greater risks, including pregnant people and those with chronic disease. Widespread exposure to microplastics complicates risk management. The policy stakes therefore extend beyond individual clinical care.
Scope of Exposure
Microplastics originate from degraded plastics, synthetic textiles, packaging, and tire wear. People ingest and inhale particles through food, water, air, and dust. Indoor environments contribute significant exposures through textiles and consumer products. Treatment systems remove some particles, but many persist. Ubiquity ensures exposures occur across communities and workplaces.
Exposure profiles can differ by occupation and neighborhood conditions. Waste handling and textile work may elevate contact with particles. Communities near busy roads may experience higher airborne microplastic levels. These disparities raise environmental justice concerns. They also inform targeted protection strategies and monitoring.
Policy Debate Ignites
The findings intensify debates over microplastic regulations and product design. Advocates call for limits on plastic additives with endocrine activity. Regulators consider standards for particle emissions and environmental monitoring. Industry stakeholders emphasize uncertainty and feasibility concerns. Negotiations now balance precaution, innovation, and economic impacts.
Regulatory Pathways Under Consideration
Agencies may integrate microplastics into existing chemical risk frameworks. Options include mandatory testing, labeling, and exposure reduction targets. Waste policies could curb fragmentation and environmental release through design changes. Procurement rules can favor lower‑shedding materials and safer additives. Standards bodies may harmonize testing and reporting methods.
Water and wastewater regulations could add particle monitoring requirements. Food contact materials may face stricter migration limits. Air quality programs could assess indoor microplastic contributions. Occupational standards might address high‑risk settings more directly. Coordinated action can improve efficiency and clarity for stakeholders.
Industry and Innovation Responses
Manufacturers explore alternative materials and coating technologies that shed fewer particles. Filtration solutions advance for water treatment, appliances, and industrial processes. Analytical tools improve detection of smaller particles and additives. Supply chains assess polymer choices and additive profiles. Market incentives could accelerate safer designs and transparency.
Interpreting the Evidence Carefully
The study reports associations rather than proven causation. Yet, consistency with mechanistic knowledge increases concern. Effect sizes appear modest but potentially meaningful across populations. Dose‑response patterns suggest plausible biological gradients. Nonlinear responses, common in endocrinology, may complicate simple threshold assumptions.
Evidence synthesis should combine epidemiology, toxicology, and exposure science. Systematic reviews can assess the weight of evidence. Transparent criteria reduce bias and improve policy credibility. Regular updates can incorporate emerging findings and methods. This approach supports adaptive, science‑based decisions.
What Individuals Can Do Now
Individual actions cannot replace systemic policy. They can still reduce exposures while policy evolves. People can limit plastic contact with hot foods and acidic beverages. Ventilation and regular dust removal can reduce indoor particle inhalation. High‑quality water filters may reduce particle levels in drinking water.
Understanding Personal Risk
The study identifies associations, not diagnoses. Hormone levels vary naturally across time and context. Individuals should discuss concerns with healthcare professionals. Clinicians can consider exposure history alongside established health guidelines. Decisions should reflect balanced evidence and personal values.
Research Priorities Ahead
Researchers need longitudinal cohorts to clarify cause and effect. Standardized methods are critical for comparability. Studies should evaluate mixtures and co‑exposures with other pollutants. Nanoplastics require special focus due to potential tissue penetration. Vulnerable populations deserve targeted investigation and protections.
Measurement and Methods Development
Harmonized sampling and laboratory protocols will reduce bias. Reference materials can improve calibration across laboratories. Noninvasive biomarkers would enable larger, more diverse studies. Advances in imaging and mass spectrometry may reveal smaller particle dynamics. Open data practices can accelerate replication and synthesis.
Mechanistic Studies and Thresholds
Experimental models can illuminate dose thresholds for endocrine effects. Studies should examine additive interactions and particle surface chemistries. Immune, microbiome, and endocrine interactions need integrated analysis. Systems biology approaches can map disruptions across tissues. Identifying reversible effects will guide interventions and policies.
Communicating Uncertainty and Action
Effective communication must present findings clearly and honestly. Audiences need context, limitations, and practical steps. Overstatement can erode trust and stall constructive policy. Transparency can support adaptive management as evidence evolves. Coordinated messaging from agencies, researchers, and clinicians will help.
Equity and Environmental Justice Considerations
Microplastic exposures can track with environmental and occupational inequities. Communities near waste facilities may face higher burdens. Workers in textiles and recycling may experience elevated exposures. Policies should include protections and monitoring in affected areas. Equity considerations strengthen public trust and effectiveness.
Economic and Health System Implications
Endocrine disruptions can contribute to downstream healthcare costs. Productivity impacts may emerge from metabolic and reproductive effects. Early prevention often costs less than later treatment. Businesses benefit from predictable, science‑based regulations. Health systems can integrate exposure screening into preventive care.
Bottom Line
The new study links microplastic exposure with measurable hormonal changes in adults. Evidence remains early, yet increasingly concerning. Policy discussions should advance with precaution and proportionality. Research must close key gaps while action reduces avoidable exposures. The public deserves clear information and practical protection.