3D-Printed Heart Tissue Patches Advance Cardiac Repair in Preclinical Models
Scientists are 3D-printing functional human heart tissue patches that repair damage in preclinical tests. These engineered patches aim to regenerate muscle lost after a heart attack and stabilize weakened heart walls. Traditional treatments reduce symptoms and slow decline but cannot replace dead heart tissue. Surgeons can bypass blocked arteries, yet scarred muscle still limits pump performance. Regenerative patches address this gap by delivering living cells and supportive scaffolds directly to injured myocardium.
Heart disease remains a leading cause of death, and post-infarction damage drives chronic heart failure. Scar tissue replaces living muscle and disrupts electrical conduction across the ventricle. Drug therapies help manage pressure and volume but do not rebuild muscle fibers. Transplants can restore function but face donor shortages and lifelong immunosuppression. These hurdles motivate targeted strategies that rebuild tissue architecture and reconnect electrical networks.
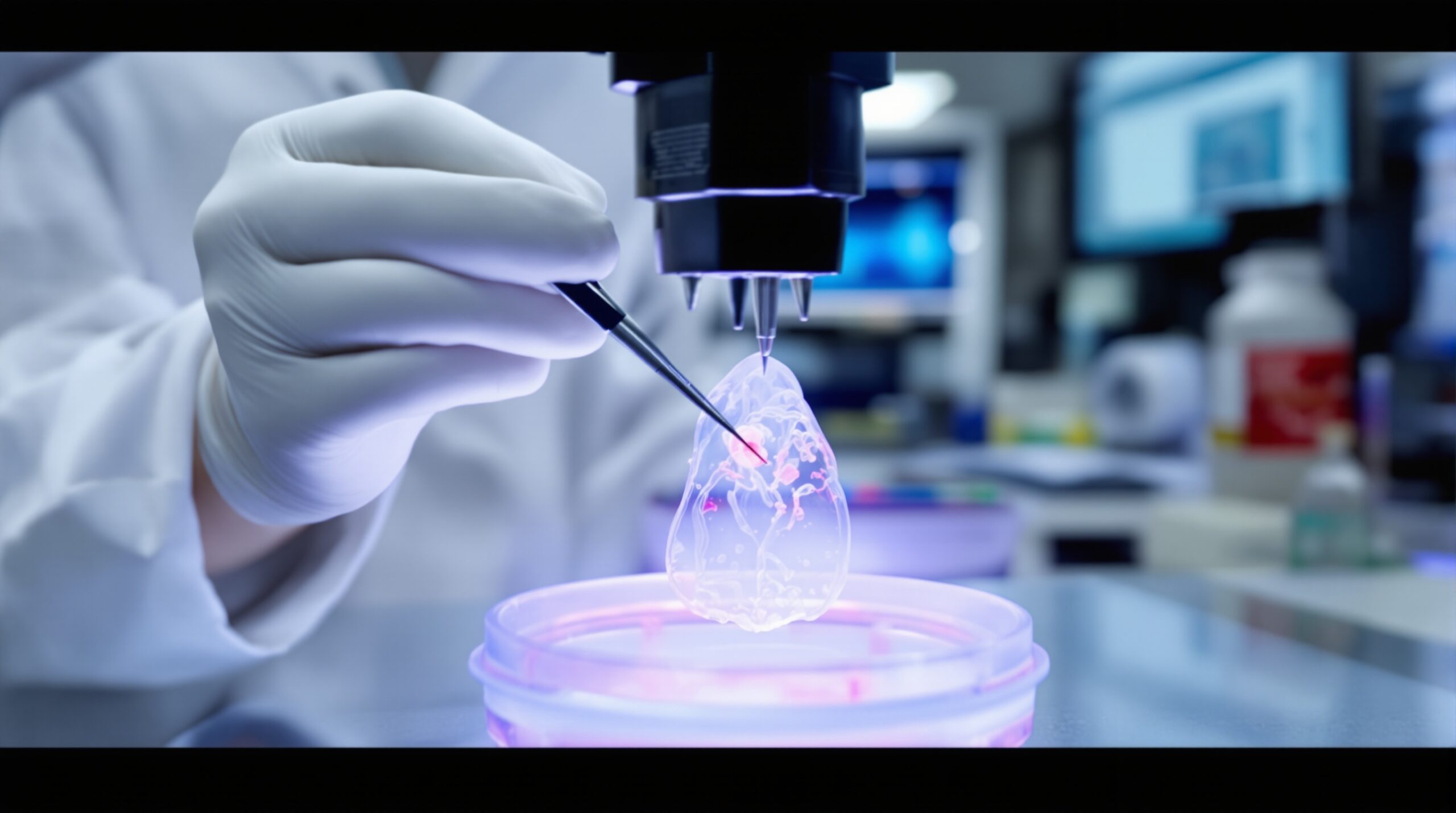
How Bioprinted Patches Are Built
Researchers use bioinks containing cells and biomaterials to print structured, living patches. The biomaterials often include hydrogels that mimic extracellular matrix and support nutrient diffusion. Common hydrogels include gelatin methacrylate, collagen, fibrin, and decellularized matrix components. Scientists suspend cardiomyocytes, fibroblasts, and endothelial cells within these supportive networks. They tailor the composition to promote stability, electrical coupling, and vascular integration after implantation.
Many teams print patches with spatially organized cell lanes and microchannels. These patterns encourage aligned muscle fibers and predictable conduction pathways across the construct. Engineers also incorporate conductive or anisotropic features to guide electrical signals. These design choices help the patch beat synchronously with host myocardium after engraftment. The goal is robust force generation without inducing arrhythmias or conduction blocks.
Printing Strategies and Design Considerations
Different printing modalities balance precision and cell survival. Extrusion bioprinting offers accessible hardware and handles viscous bioinks well. Stereolithography and digital light processing can create finer features with photopolymerizable materials. Coaxial printing enables microchannels for perfusion and vascular templating. Each strategy manages trade-offs between resolution, speed, and biological viability.
Engineers tune stiffness and elasticity to match native ventricular tissue. Mechanical compatibility reduces stress concentrations at the patch boundary. Designers also consider thickness and diffusion limits that affect oxygen delivery. Multilayer constructs may include perfusable channels or embedded vascular networks. These elements sustain cells in thicker tissues before host vessels grow in.
Functional Integration With Host Tissue
Successful patches must electrically integrate with surrounding myocardium. Conductive pathways and gap junction proteins support synchronized contraction across the graft. Researchers encourage this by maturing cardiomyocytes in bioreactors with electrical pacing. Mechanical conditioning also improves alignment and force generation. Together, these conditioning steps reduce arrhythmic risks after implantation.
Vascularization remains another critical requirement. Endothelial cells within printed channels form primitive vessels before implantation. After placement, host capillaries infiltrate and connect with these microvascular structures. Pre-vascularized patches usually show better cell survival and function. Enhanced perfusion supports long-term integration and resistance to ischemic stress.
Evidence From Preclinical Tests
Multiple preclinical studies report functional recovery after patch implantation. Animal models of myocardial infarction show reduced scar burden and improved contractile performance. Echocardiography and pressure measurements commonly demonstrate better pump function. Histology often reveals new vessels within the patch and border zone. Importantly, implanted patches generally maintain structural integrity during cardiac cycles.
Small animal models help optimize composition, architecture, and delivery techniques. Large animal studies assess surgical feasibility and safety in clinically relevant settings. Surgeons evaluate suturing strategies, patch fixation, and hemodynamic stability during placement. Investigators monitor rhythm, inflammation, and immune responses after implantation. These studies inform clinical protocols and risk mitigation plans.
Cell Sources and Maturation Strategies
Human induced pluripotent stem cells supply patient-specific cardiomyocytes and endothelial cells. These cells enable autologous or immuno-matched therapies when feasible. Some approaches use allogeneic cell banks for scalability and consistency. Researchers differentiate cardiomyocytes, then culture them to enhance maturity. Electrical pacing and metabolic conditioning promote adult-like electrophysiology and contractility.
Mixed cell populations can improve outcomes. Fibroblasts contribute extracellular matrix and mechanical stability. Endothelial cells and perivascular cells support rapid vessel formation. These combinations foster a microenvironment that mirrors native heart tissue. Balanced proportions help reduce arrhythmias and support coordinated beating.
Manufacturing and Quality Control
Translational efforts require rigorous manufacturing controls. Teams produce bioinks under sterile, validated conditions. Batch-to-batch consistency is essential for clinical reproducibility. Potency assays evaluate electrical activity, force generation, and conduction velocity. Release criteria also include sterility, viability, and mechanical performance metrics.
Bioreactors provide controlled environments for conditioning and maturation. Sensors track pH, oxygen, and contractile behavior during culture. Automation reduces variability and operators’ exposure to open processes. Documentation supports traceability from source materials to finished patches. This infrastructure aligns with good manufacturing practice requirements.
Safety, Ethics, and Regulatory Pathways
Regulators consider printed patches as combination products with device and biologic elements. Developers engage early with regulatory agencies to define testing plans. Safety assessments evaluate arrhythmia risk, thrombogenicity, and inflammatory responses. Long-term studies track patch durability and potential calcification. Investigators also monitor for ectopic tissue formation and tumorigenicity.
Ethical considerations include donor cell sourcing and informed consent for stem cell lines. Patient-specific approaches raise privacy and data security considerations. Teams implement identity controls for cell lines and derived products. Governance frameworks address equitable access as technologies mature. Clear communication builds public trust and supports responsible deployment.
Comparison With Alternative Approaches
Cell injections deliver dispersed cells but often show limited retention. Printed patches provide structural support and defined architecture. Decellularized tissue patches offer scaffolding but lack robust contractile elements. Gene therapies modify pathways but do not directly replace lost muscle. Mechanical devices unload the heart but require long-term management.
3D-printed patches integrate the advantages of cells and scaffolds. They deliver aligned muscle fibers and preformed microvasculature. Their design enables tailored mechanics for individual patient needs. Engineers can scale dimensions to fit specific infarct sizes. This flexibility supports personalized surgical planning and targeted repair.
Clinical Delivery and Surgical Considerations
Cardiac surgeons typically place patches on the epicardial surface over infarct zones. Sutures or bioadhesives secure the construct in place. Teams evaluate minimally invasive approaches for select anatomies. Imaging guides placement and confirms contact with healthy border myocardium. Postoperative care monitors rhythm, function, and inflammatory markers.
Anesthesiologists and perfusionists manage hemodynamics during patch placement. Coordination reduces ischemic time and supports stable conditions. Surgeons consider pericardial constraints and potential adhesions. Biocompatible adhesives may shorten operative time in appropriate cases. These tactics streamline procedures and reduce risks.
Remaining Challenges
Thick tissues still face diffusion limits without robust vascular networks. Researchers refine microchannel designs to enhance perfusion. Achieving adult-like cardiomyocyte maturity remains difficult in vitro. Teams test metabolic switches to favor oxidative phosphorylation and improved calcium handling. Electromechanical integration also requires precise mapping and pacing strategies.
Durability under continuous contraction is another key concern. Materials must withstand billions of cardiac cycles. Designers study fatigue behavior and long-term mechanical stability. Biodegradable components should degrade at clinically appropriate rates. Matching degradation to tissue remodeling improves outcomes.
Scaling, Cost, and Access
Manufacturing scale influences cost and availability. Allogeneic platforms can reduce production time and expense. Automation and closed systems improve throughput and consistency. Health systems evaluate cost effectiveness relative to advanced heart failure treatments. Payers will require long-term outcome data for reimbursement decisions.
Training programs will expand the pool of qualified operators. Standardized protocols ease technology transfer between centers. Professional societies can publish consensus recommendations. Shared registries will capture safety and effectiveness data. These steps accelerate responsible clinical adoption.
Toward First-in-Human Studies
Translational teams plan early feasibility trials with carefully defined endpoints. Primary outcomes often include safety and procedural success. Secondary measures examine functional recovery and quality of life. Imaging and electrophysiology provide objective assessments of integration. Careful patient selection supports clear signal detection.
Regulators may request staged enrollment with independent monitoring. Investigators will publish transparent outcomes and adverse event reports. These data will guide design improvements and dosing strategies. Success will depend on comprehensive follow-up and multidisciplinary collaboration. Lessons will inform broader pivotal trials and real-world use.
Outlook for Cardiac Regeneration
3D-printed heart tissue patches show compelling promise in preclinical models. They address core barriers limiting conventional therapies. Engineers continue improving vascularization, maturity, and mechanical integration. Clinicians refine delivery strategies and patient selection criteria. Regulators and manufacturers coordinate to ensure quality and safety.
Continued progress will depend on rigorous science and careful translation. Partnerships across academia, industry, and health systems will be essential. Evidence-based adoption will protect patients and sustain public trust. With thoughtful development, printed patches could transform myocardial repair. The path ahead is challenging but increasingly well charted.